Interventions
Preconception care should be the earliest part of an interconnected chain of subsequent prenatal, neonatal, child, and youth care. Preconception care requires the involvement of health authorities, NGOs, and many healthcare disciplines such as general practitioners, midwives, obstetricians, paediatricians, clinical geneticists, community healthcare workers and other maternal and child health professionals.
The core components of preconception care consist of health promotion, risk assessment, and specific interventions. Some approaches target the general population at large, some focus on both future parents individually, and others on all women of reproductive age:
-
Collective measures are aimed at the general population to improve preconception health. Examples include radiological protection of all women of reproductive age, cigarette package labelling to prevent low birth weight in singletons, and educational campaigns on the use of folic acid.
-
General individual preconception care is provided by primary care workers to all couples planning pregnancy. Community healthcare workers can reach people through their networks with information promoting healthy behaviour and preventive actions (e.g., individual advice on smoking cessation). By informing people about the importance of preconception care, they can stimulate demand for appropriate services. They can act as a link between the community or broader population and formal healthcare services.
-
Specialized individual preconception care is provided to:
a) couples already known to be at risk for adverse pregnancy outcomes (e.g., due to prior pregnancy complications or chronic illness), or
b) couples referred from general individual preconception care after risk assessment (including medication use, genetic disorders in the family, or specific working conditions of women).
Health policy, guidelines and multidiciplinary care pathways for the provision of preconception should take into account the following aspects::
- standardized risk assessment tools;
- training of professionals;
- standardized communication tools and strategies adaptable to local contexts;
- clear distribution of tasks and responsibilities among professionals providing individual care;
- involvement of municipal public health institutions, schools, employers, etc.
Missing link?
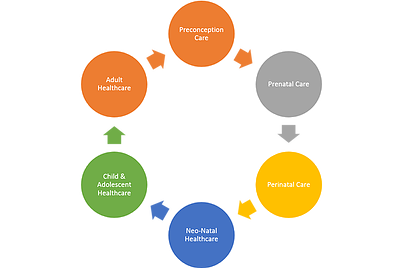
Worldwide, preconception should be the additional link in a continuum of maternal, prenatal, newborn and child health, with the goal of enabling healthy longevity.
The "Current" Continuum of Care
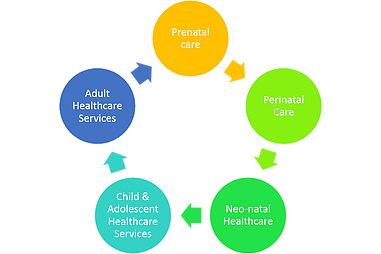
Continuum of Care Model - With missing link "Preconception Care"